Drug Information
| Drug General Information | Top | |||
|---|---|---|---|---|
| Drug ID |
D0O1WX
|
|||
| Former ID |
DAP001465
|
|||
| Drug Name |
Ciprofloxacin XR
|
|||
| Synonyms |
ciprofloxacin; 85721-33-1; Ciprofloxacine; Ciprobay; Ciproxan; Ciprofloxacina; Ciprofloxacinum; Ciprofloxacino; Cipro IV; Ciproxina; Ciprinol; Bernoflox; Ciprodar; Cifloxin; Septicide; Bacquinor; Ciproquinol; Cipromycin; Ciprocinol; Cipro XR; Superocin; Ciprowin; Ciprolon; Ciproflox; Ciprecu; BAY q 3939; Spitacin; Quintor; Quinolid; Proflaxin; Probiox; Ipiflox; Zumaflox; Ciproxine; Ciprolin; Roxytal; Italnik; Fimoflox; Corsacin; Citopcin; Ciprogis; Rancif; Ciriax; Ciplus; Baflox; Loxan; Cilab; Cycin; Cixan; Unex; GW1843; Ciprofloxacin Hydrochloride; Ciprofloxacin intratympanic - Otonomy
Click to Show/Hide
|
|||
| Drug Type |
Small molecular drug
|
|||
| Indication | Bacterial infection [ICD-11: 1A00-1C4Z; ICD-10: A00-B99] | Approved | [1] | |
| Gram-positive bacterial infection [ICD-11: 1B74-1G40] | Approved | [2] | ||
| Cystic fibrosis [ICD-11: CA25; ICD-10: E84, E84.9; ICD-9: 277] | Phase 2 | [3] | ||
| Biliary cancer [ICD-11: 2E92.7; ICD-10: D13.4] | Phase 1 | [4] | ||
| Company |
Depomed Bayer
|
|||
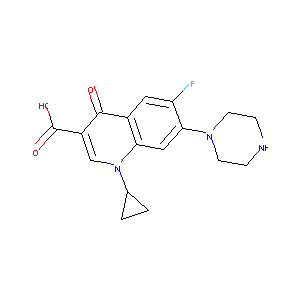
| Structure |
 |
Download2D MOL |
||
| Formula |
C17H18FN3O3
|
|||
| Canonical SMILES |
C1CC1N2C=C(C(=O)C3=CC(=C(C=C32)N4CCNCC4)F)C(=O)O
|
|||
| InChI |
1S/C17H18FN3O3/c18-13-7-11-14(8-15(13)20-5-3-19-4-6-20)21(10-1-2-10)9-12(16(11)22)17(23)24/h7-10,19H,1-6H2,(H,23,24)
|
|||
| InChIKey |
MYSWGUAQZAJSOK-UHFFFAOYSA-N
|
|||
| CAS Number |
CAS 85721-33-1
|
|||
| PubChem Compound ID | ||||
| PubChem Substance ID |
854234, 7849275, 8188389, 12012611, 14780446, 43120033, 50065329, 50125725, 57314943, 80847453, 81043820, 85174197, 92722913, 93305520, 99319459, 104327163, 115354412, 118836555, 125358728, 126603656, 126617874, 126653698, 126663877, 131328379, 131549783, 134338664, 135019641, 143449628, 143837408, 162251668, 163370746, 164788124, 165235301, 175267218, 175611737, 196107810, 223683480, 226414707, 249857489, 252427178
|
|||
| ChEBI ID |
CHEBI:100241
|
|||
| ADReCS Drug ID | BADD_D00471 ; BADD_D00472 | |||
| Interaction between the Drug and Microbe | Top | |||
|---|---|---|---|---|
| The Abundace of Studied Microbe(s) Regulated by Drug | ||||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Bacillales | ||||
|
Studied Microbe: Staphylococcus
Show/Hide Hierarchy
|
[5] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Staphylococcus was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Bacteroidales | ||||
|
Studied Microbe: Alistipes
Show/Hide Hierarchy
|
[6] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | C57BL/6 mice | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Alistipes was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Alistipes
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Alistipes was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Bacteroides
Show/Hide Hierarchy
|
[6] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | C57BL/6 mice | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Bacteroides was increased by Ciprofloxacin. | |||
|
Studied Microbe: Bacteroides
Show/Hide Hierarchy
|
[8] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Bacteroides was increased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Bifidobacteriales | ||||
|
Studied Microbe: Bifidobacterium
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Bifidobacterium was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Gardnerella
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Gardnerella was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Burkholderiales | ||||
|
Studied Microbe: Sutterella
Show/Hide Hierarchy
|
[10] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Sutterella was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Enterobacterales | ||||
|
Studied Microbe: Citrobacter
Show/Hide Hierarchy
|
[11] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Citrobacter was increased by Combination of ciprofloxacin and clindamycin. | |||
|
Studied Microbe: Citrobacter
Show/Hide Hierarchy
|
[12] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Cirrhosis | |||
| Description | The abundance of Citrobacter was increased by Ciprofloxacin. | |||
|
Studied Microbe: Enterobacter
Show/Hide Hierarchy
|
[12] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Cirrhosis | |||
| Description | The abundance of Enterobacter was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Enterobacter
Show/Hide Hierarchy
|
[13] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Enterobacter was increased by Ciprofloxacin. | |||
|
Studied Microbe: Escherichia
Show/Hide Hierarchy
|
[8], [14] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Escherichia was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Escherichia coli
Show/Hide Hierarchy
|
[15] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Escherichia coli was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Klebsiella
Show/Hide Hierarchy
|
[12] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Cirrhosis | |||
| Description | The abundance of Klebsiella was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Erysipelotrichales | ||||
|
Studied Microbe: Holdemania
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Holdemania was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Eubacteriales | ||||
|
Studied Microbe: Blautia
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Blautia was increased by Ciprofloxacin. | |||
|
Studied Microbe: Clostridium
Show/Hide Hierarchy
|
[5] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Clostridium was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Clostridium
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Clostridium was increased by Ciprofloxacin. | |||
|
Studied Microbe: Clostridium difficile
Show/Hide Hierarchy
|
[16] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Clostridium difficile was not significantly changed by Ciprofloxacin. | |||
|
Studied Microbe: Coprococcus
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Coprococcus was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Eubacterium
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Eubacterium was increased by Ciprofloxacin. | |||
|
Studied Microbe: Faecalibacterium
Show/Hide Hierarchy
|
[8] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Faecalibacterium was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Faecalibacterium
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Faecalibacterium was not significantly changed by Ciprofloxacin. | |||
|
Studied Microbe: Roseburia
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Roseburia was increased by Ciprofloxacin. | |||
|
Studied Microbe: Ruminococcaceae
Show/Hide Hierarchy
|
[8] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Ruminococcaceae was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Ruminococcus
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Ruminococcus was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Fusobacteriales | ||||
|
Studied Microbe: Fusobacterium
Show/Hide Hierarchy
|
[15] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Fusobacterium was not significantly changed by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Lactobacillales | ||||
|
Studied Microbe: Enterococcus
Show/Hide Hierarchy
|
[11] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Enterococcus was increased by Combination of ciprofloxacin and clindamycin. | |||
|
Studied Microbe: Lactobacillus
Show/Hide Hierarchy
|
[12] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Cirrhosis | |||
| Description | The abundance of Lactobacillus was not significantly changed by Ciprofloxacin. | |||
|
Studied Microbe: Lactobacillus
Show/Hide Hierarchy
|
[5] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Lactobacillus was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Streptococcus
Show/Hide Hierarchy
|
[5] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Streptococcus was decreased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Pseudomonadales | ||||
|
Studied Microbe: Pseudomonas
Show/Hide Hierarchy
|
[12] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Cirrhosis | |||
| Description | The abundance of Pseudomonas was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Pseudomonas
Show/Hide Hierarchy
|
[16] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Pseudomonas was not significantly changed by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Veillonellales | ||||
|
Studied Microbe: Dialister
Show/Hide Hierarchy
|
[9] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Urinary tract infection | |||
| Description | The abundance of Dialister was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Veillonella
Show/Hide Hierarchy
|
[5] | |||
| Hierarchy | ||||
| Abundance Change | Decrease | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Veillonella was decreased by Ciprofloxacin. | |||
|
Studied Microbe: Veillonella
Show/Hide Hierarchy
|
[15] | |||
| Hierarchy | ||||
| Abundance Change | Increase | |||
| Experimental Species | Human | Experimental Sample | Saliva | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Veillonella was increased by Ciprofloxacin. | |||
| The Order in the Taxonomic Hierarchy of the following Microbe(s): Verrucomicrobiales | ||||
|
Studied Microbe: Akkermansia
Show/Hide Hierarchy
|
[7] | |||
| Hierarchy | ||||
| Abundance Change | No significant change | |||
| Experimental Species | Human | Experimental Sample | Faeces | |
| Disease or Condition | Healthy | |||
| Description | The abundance of Akkermansia was not significantly changed by Ciprofloxacin. | |||
| References | Top | |||
|---|---|---|---|---|
| REF 1 | Drugs@FDA. U.S. Food and Drug Administration. U.S. Department of Health & Human Services. 2015 | |||
| REF 2 | Emerging drugs for bacterial urinary tract infections. Expert Opin Emerg Drugs. 2005 May;10(2):275-98. | |||
| REF 3 | Inhaled Ciprofloxacin for the Management of Infections in Non-Cystic Fibrosis Bronchiectasis (BE) Patients | |||
| REF 4 | Low folate conditions may enhance the interaction of trifluorothymidine with antifolates in colon cancer cells. Cancer Chemother Pharmacol. 2006 Jan;57(2):171-9. | |||
| REF 5 | Influence of ciprofloxacin on the colonic microflora in young and elderly volunteers: no impact of the altered drug absorption. Scand J Infect Dis. 1990;22(2):205-8. | |||
| REF 6 | Antibiotic-Induced Alterations of the Murine Gut Microbiota and Subsequent Effects on Colonization Resistance against Clostridium difficile. mBio. 2015 Jul 14;6(4):e00974. | |||
| REF 7 | Same Exposure but Two Radically Different Responses to Antibiotics: Resilience of the Salivary Microbiome versus Long-Term Microbial Shifts in Feces. mBio. 2015 Nov 10;6(6):e01693-15. | |||
| REF 8 | Determining the Long-term Effect of Antibiotic Administration on the Human Normal Intestinal Microbiota Using Culture and Pyrosequencing Methods. Clin Infect Dis. 2015 May 15;60 Suppl 2:S77-84. | |||
| REF 9 | Collateral damage from oral ciprofloxacin versus nitrofurantoin in outpatients with urinary tract infections: a culture-free analysis of gut microbiota. Clin Microbiol Infect. 2015 Apr;21(4):344.e1-11. | |||
| REF 10 | Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 2011 Mar 15;108 Suppl 1(Suppl 1):4554-61. | |||
| REF 11 | Influence of low dose ciprofloxacin on microbial colonization of the digestive tract in healthy volunteers during normal and during impaired colonization resistance. Scand J Infect Dis. 1997;29(3):297-300. | |||
| REF 12 | Efficacy of oral ciprofloxacin as selective intestinal decontaminant in cirrhosis. Ital J Gastroenterol Hepatol. 1997 Jun;29(3):262-6. | |||
| REF 13 | Changes in the pharmacokinetics of ciprofloxacin and fecal flora during administration of a 7-day course to human volunteers. Antimicrob Agents Chemother. 1984 Nov;26(5):757-61. | |||
| REF 14 | Quinolones and colonization resistance in human volunteers. Pharm Weekbl Sci. 1986 Feb 21;8(1):67-71. | |||
| REF 15 | Impact of Ciprofloxacin and Clindamycin Administration on Gram-Negative Bacteria Isolated from Healthy Volunteers and Characterization of the Resistance Genes They Harbor. Antimicrob Agents Chemother. 2015 Aug;59(8):4410-6. | |||
| REF 16 | Effect of oral ciprofloxacin on the faecal flora of healthy volunteers. Eur J Clin Microbiol. 1986 Apr;5(2):201-5. | |||
| REF 17 | Drugs@FDA. U.S. Food and Drug Administration. U.S. Department of Health & Human Services. | |||
| REF 18 | DOI: 10.1093/jac/48.4.479 | |||
| REF 19 | Loss of folylpoly-gamma-glutamate synthetase activity is a dominant mechanism of resistance to polyglutamylation-dependent novel antifolates in multiple human leukemia sublines. Int J Cancer. 2003 Feb 20;103(5):587-99. | |||
If You Find Any Error in Data or Bug in Web Service, Please Kindly Report It to Dr. Zhou and Dr. Zhang.

